In modern healthcare, rehabilitation and allied health services play a vital role in helping patients regain function, independence, and quality of life after illness, injury, or surgery.
These services encompass a wide range of therapies—including physiotherapy, occupational therapy, and speech pathology—that are delivered by trained allied health professionals. Together, they support a holistic recovery process tailored to each patient’s unique needs.
Integrating these services directly within a healthcare facility is not only convenient for patients but also critical for providing coordinated, continuous care.
A well-planned allied health unit layout ensures seamless collaboration between clinical teams, reduces patient transfer times, and improves access to essential therapies.
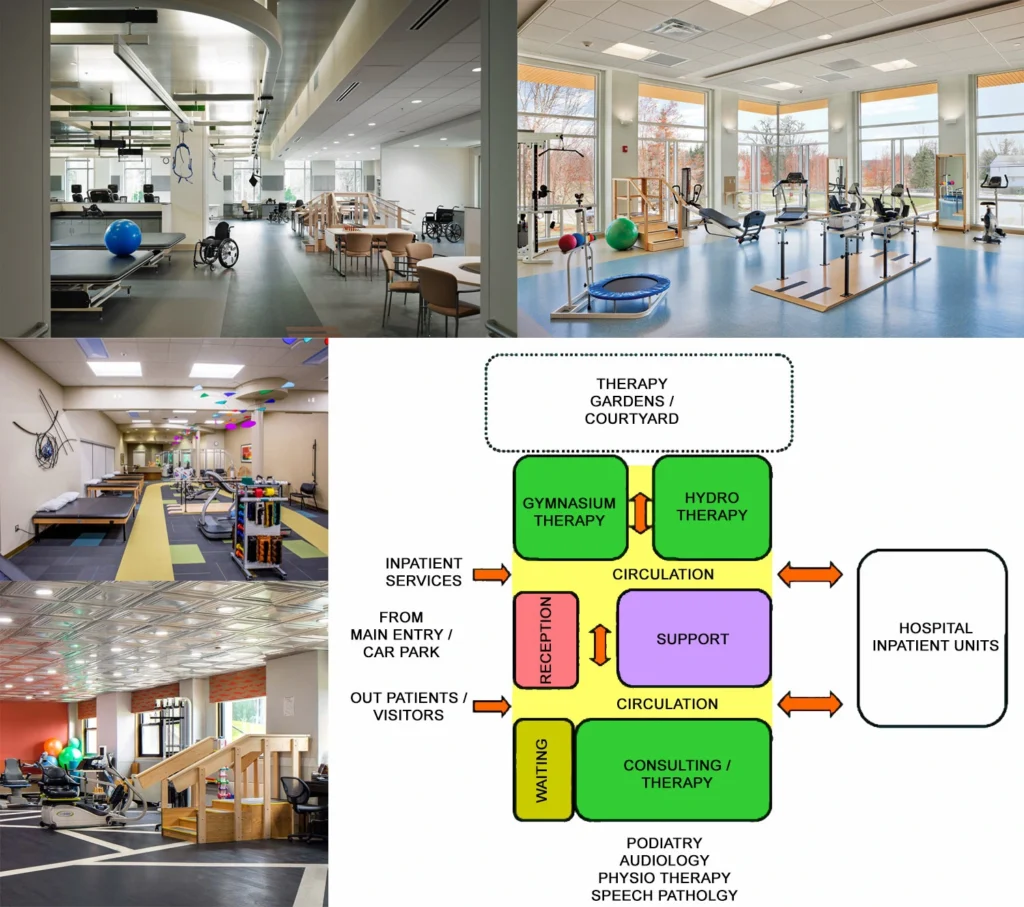
The design of a rehabilitation space has a profound impact on both patient outcomes and operational efficiency. Elements such as room configuration, accessibility, natural lighting, and the proximity of therapy zones to patient wards all influence how care is delivered and experienced.
As a result, rehabilitation design has become a core focus of healthcare facility planning, with growing attention on creating environments that support recovery, safety, and staff well-being.
If you want to know about the Types of slabs or Permeable concrete or Islamic architecture, please click the link.
1) Introduction
The Rehabilitation – Allied Health Unit provides a multi disciplinary rehabilitation service care in which the clinical intent or treatment goal is to improve the functional status of a patient with an impairment, disability or handicap.
Facilities for Physiotherapy and Occupational Therapy will vary greatly, ranging from large, purpose-designed, central facilities for inpatients and/or outpatients, to basic on-ward or bedside services.
Extent, design and location of facilities will be affected by presence or otherwise of the following services (not inclusive):
- Rehabilitation Medicine
- Aged Care
- Spinal Cord Injury Service
- Orthopaedic Services
- Neurosciences – (Strokes, Multiple Sclerosis, Traumatic Brain Injuries etc)
- Amputees
- Hand Surgery / Plastic Services.
Speech Pathology plays a major role in Neonatal, Paediatric, ENT / Maxillofacial and neurological services; in the absence of these, Speech Pathology may be provided on a parttime basis. Children’s Hospitals or major Paediatric Services generate their own specific spatial needs.
At higher Role Delineation levels it is possible that each discipline may have its own discrete department but every attempt should be made to co-locate the therapy units to maximise the potential for sharing and to facilitate multidisciplinary care.
The rehabilitation services will be supported by full time Social Work services. At Level 4, Dietetics and Podiatry are generally provided as part time services and can be incorporated into the Unit.
At Levels 5 & 6 they will have their own discrete Units and are excluded from the Schedule of Accommodation at those levels.
Clinical Psychology and Neuropsychology also play an important role in some aspects of service provision and will need their own or access to office/treatment areas.
i) Patient Characteristics
All ages from children to the frail aged may be treated. Almost all patients attending for physiotherapy are physically incapacitated to some extent many of whom use wheelchairs or walking aids and – increasingly – motorised chairs that have implications for parking and recharging.
Many patients may be disfigured (burns, throat surgery etc) and require a nonthreatening, private environment. Patients may require access to interpreter services.
2) Planning of Rehabilitation – Allied Health Unit
i) Operation Models
Hours of Operation
The Unit will generally operate during business hours Monday to Friday with after-hours oncall physiotherapy services available for inpatient units as required. Some departments may provide a limited service at evenings and weekends.
If used for health education classes (e.g. antenatal classes), after-hours access will be required. If a hydrotherapy pool is part of the facility, this too may be made available to the community after hours and at week-ends and therefore careful consideration will need to be given to location, controlled access and security.
Flexibility
The facilities of the Unit will be utilised by inpatients and outpatients. It is expected that the majority of inpatients accommodated in the Rehabilitation Inpatient Unit will attend the Unit on a daily basis.
The function of these two units is inter-related and the design of the Rehabilitation Unit could provide areas common to both units. As with other areas of health care, rehabilitation services are constantly evolving.
This is manifest in terms of:
- Clinical development – many more categories of patient are able to be rehabilitated than was previously considered feasible
- Organisational development – the interrelationship of the various medical, nursing and allied health services that participate in the rehabilitation process is of paramount importance
- Technological development – advances in technology have developed techniques which will ultimately become routine aspects of rehabilitation. Such developments include kinematic analysis, electromyography and ergometry.
Models of Care
Traditionally the model of care has been one-to-one, therapist to patient. Increasingly an educative model is being used that assumes a staff to patient ratio of 1:4 or more and incorporates:
- Group sessions for peer support;
- Group exercise classes;
- Involvement of carers so that they can learn how much activity the patients can safely tolerate at home and how best to support them;
- Education programmes.
There may need to be separate areas for Respiratory and Cardiac Rehabilitation and general rehabilitation as the patients have differing needs and sometimes equipment. However this will depend on the number of sessions and every opportunity should be made to share areas between programmes.
Satellite Units
One of the problems of providing therapy services for inpatients within the Unit itself is transport to and from hospital units, particularly, for example, neuroscience patients whose attention span may be limited and who need a quiet environment. It also requires either a portering service or use of valuable therapist time in transport functions.
If distance from inpatient units to the Rehabilitation therapy areas is considerable and throughput can justify, provision of a small satellite unit may be considered – mainly for physiotherapy – near the units most affected, usually Neuroscience & Orthopaedics. Or alternatively, a small therapy / multipurpose room in an inpatient unit may serve such a purpose.
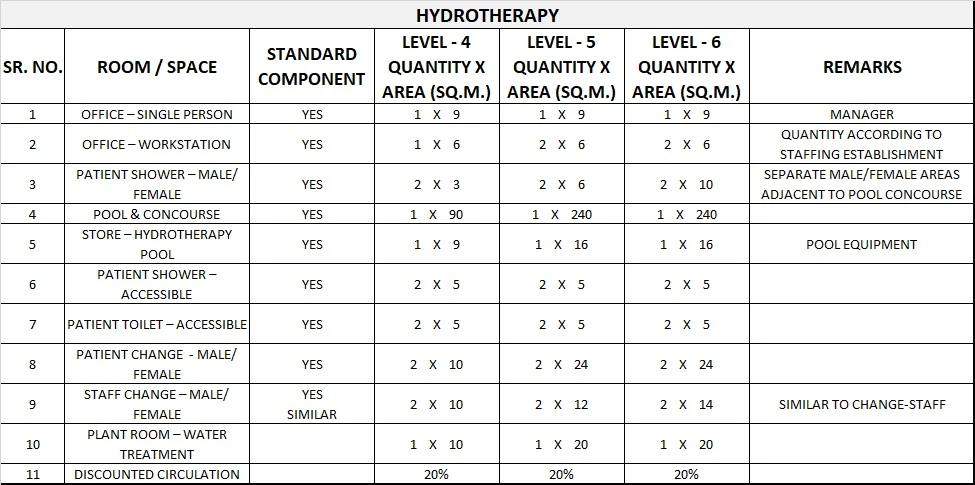
Hydrotherapy
Whilst there are differing opinions as to the therapeutic benefits of hydrotherapy, a designated Rehabilitation service will probably require access to a hydrotherapy pool.
However, in other circumstances, the need for a pool should be carefully considered as the cost per unit of treatment is high and conditions for which hydrotherapy is the only appropriate treatment are limited.
Hydrotherapy pools should only be provided where patient numbers can be justified and where the pool is required for a minimum of four hours each days, five days a week.
Utilisation of the pool may be extended by making the pool available to groups within the community for their use at times when it is not required for specific therapeutic purposes. Alternatively, use of a pool already established in the community may be used.
Gait Analysis Laboratory
Quantitative gait analysis is useful in objective assessment and documentation of walking ability as well as identifying the underlying causes of walking abnormalities in patients with cerebral palsy, stroke, head injury and other neuromuscular problems.
The results of gait analysis have been shown to be useful in determining the best course of treatment in these patients. Equipment for gait analysis may be incorporated into a gymnasium.
Outdoor Gait Area
It is essential to provide mobility training on a range of uneven surfaces necessary for community integration.
ii) Operational Policies
General
Depending upon the needs of the individual hospital, it may be decided that the Rehabilitation Allied Health Unit will provide the location for the hospital’s Acute Therapy Services.
If such a Policy is adopted it may be necessary to upgrade the accommodation to provide:
- Additional therapy spaces for general acute inpatient and outpatient therapy
- Additional group office space for physiotherapists to write up notes
- Additional staff amenities.
The Guideline defines functional spaces as discrete areas for defined activities. The Operational Policy of a facility may compel the design team to view the various functions and activities within the Unit from the framework of a team philosophy. Accordingly, patient flow would determine the definition of spaces rather than individual allied health discipline.
Outpatients Versus Day Patients
The original “Day Hospital” concept often accommodated patients for respite care; in modern units patients are admitted for treatment, not respite. Patients attending for a single treatment by a single therapist are classified as outpatients.
Patients attending for a series of treatments by different therapists will be admitted as day patients where stay is in excess of 4 hours. This latter category will need an area for rest and refreshment between treatments.
Medical Records & X-Rays
Assuming a hard copy system, it is usual for non-inpatient records to be kept in the Unit for the duration of treatment. For a hard copy system, x-ray viewing boxes will be required and films requested from the Medical Imaging Unit.
When records become electronic, there will be direct data entry and design should indicate likely locations for computers and allow for appropriate power and cabling. Assuming a digital PACS system, X-ray films are available on screen so viewing monitors will be needed.
Patient Lifting / Transfers
Patient handling measures may include ceiling hoist systems for transfers from wheelchair to plinth, or mobile lifters. Mobile patient lifters will require bays with power for recharging. The Gymnasium should include additional space for holding lifting devices.
Recharging of Electrical Wheelchairs
Inpatients normally using electric wheelchairs or motorised chairs may need somewhere to park and recharge their equipment whilst in hospital.
In inpatient and rehabilitation units where wheelchair use is significant, provide sufficient facilities to recharge patients’ electric wheelchairs and motorised chairs overnight including power outlets. Ideally wheelchair parking areas should not impede corridor space.
Specific Needs in Inpatient Units
To avoid unnecessary transport to and from the main unit, space and facilities for ward-based therapy could be considered. Include but not confined to:
- 10 m corridor length for walking tests
- Storage for equipment & mobility aids
- Ward-based treatment space larger than the area around a patient’s bed
- Access to stairs for practising crutches
- Access to write-up area and storage of resource material.
Staffing
The staffing operational policy assumptions made in this guideline are:
- Office space will be provided where required for clerical and allied health staff including workstations in open treatment areas for immediate documentation.
- “hot” desks will be available for students and visiting staff
- Staff wearing uniforms will arrive at the Unit in uniform however shower / change facilities will be required for comfort reasons as much of the work is labour-intensive.
The number of staff will depend on the needs of the individual hospital / service. Staff mix may include – either permanently or when required by referral:
- Director of Rehabilitation Medicine and/or the head of each therapy discipline
- Medical staff
- Nursing staff
- Physiotherapists
- Occupational therapists
- Social workers
- Speech pathologist
- Neuropsychologist (where brain impairment is an issue)
- Clinical psychologist (for treatment of complex behavioural disturbances)
- Prosthetists / Orthotists
- Aides
- Podiatrist
- Sport & Recreational Officers
- Dietitians
- Diversional Therapist
- Vocational Trainers
- Case Co-Ordinators
- Rehabilitation Engineers
- Clerical staff
- Housekeeper and cleaning staff
- Artisan and transport staff.
- Students of various disciplines
Teaching
Most units will be involved with undergraduate and / or postgraduate training. Attendance will be variable. Students will need write-up space near the area of activity and numbers will need to be ascertained. Facilities will include a workstation for the supervisor and student lockers.
Emergency Equipment
- Oxygen (wall panels or cylinders) for oxygen-dependent patients
- Cardiac monitor for cardiac patients
- Resuscitation trolley/s
- Medical gas service panels in selected locations for emergency use.
iii) Functional Areas
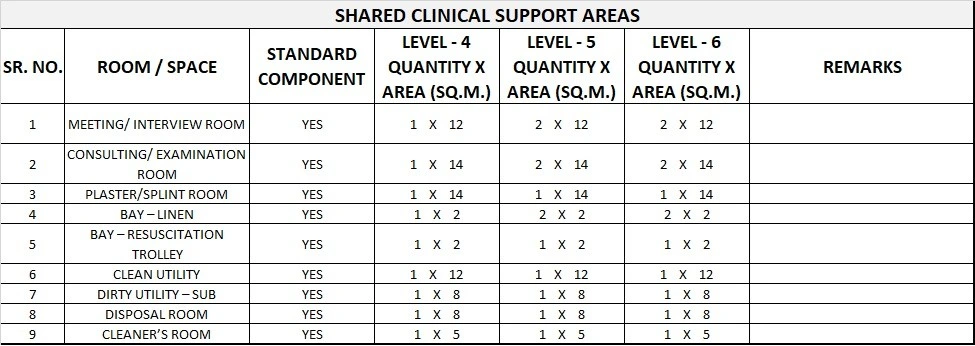
The Rehabilitation – Allied Health services may include Dietetics, Hydrotherapy, Occupational Therapy, Physiotherapy, Podiatry, Psychology, Speech Pathology, and Social Work. The Rehabilitation – Allied Health Unit will include the following Functional Areas:
- Entry, Reception and Waiting areas
- Patient accommodation areas including Lounge and Dining areas
- Patient Therapy areas which may be shared
- Support areas including Utilities, Cleaner’s Room, Disposal, Pantry and Store Rooms
- Staff areas including Offices, Meeting Rooms, Staff Change and Toilets.
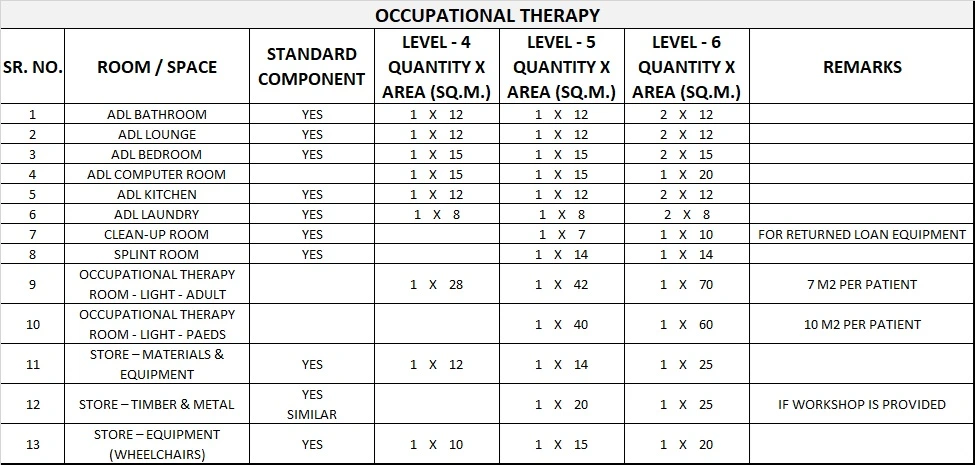
Occupational Therapy
Where an Occupational Therapy service is to be provided the following functions or facilities shall be allowed for:
- Therapy areas
- Office / Administrative areas
- Hand-washing facilities
- Availability of Accessible Toilet
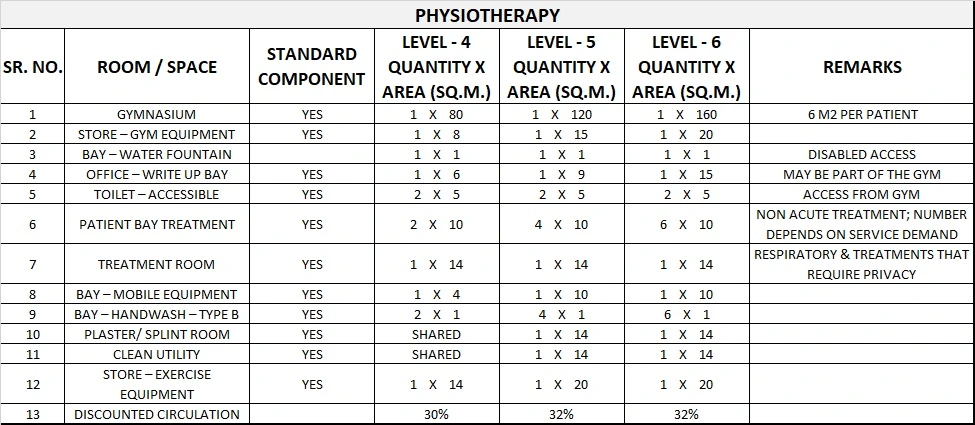
Physiotherapy
Where a Physiotherapy service is to be provided the following facilities shall be allowed for:
- Individual treatment area or areas that provide for patient privacy
- Staff hand-washing facilities close to each treatment space; this may serve several treatment spaces
- An exercise area with facilities appropriate for the level of intended service
- Clean linen storage; in the form of built-in cupboards, cabinets or on mobile storage trolleys
- Storage for equipment and supplies
- Storage for soiled linen and waste
- Patient dressing and changing with secure storage of clothing and valuables, showering and toilet facilities
- Ice-making facilities to be available in or near the department
- Wall oxygen in patient waiting areas depending on service mode, and access to appropriate outdoor therapy areas.
Entry Areas
The entry canopy is required to provide dry access to the building. Design considerations include:
- Ensuring the covered area is large enough to allow vehicles such as taxis, buses, cars, and emergency vehicles to manoeuvre beneath it, and is structured to facilitate free concurrent traffic flow for multiple vehicles
- The use of clear roofing material to maximise natural light inside the building.
The external Entrance Area, best sited at ground floor level, is the first point of contact for members of the community and should display clear directions informing people where to proceed.
Design considerations include:
- Vehicle access is required at all times
- Entry facilities should be suitable for people with disabilities, such as limited mobility and poor vision
- The entry can incorporate an airlock space and may have sensor or automatically opening doors to facilitate access.
Patient Lounge Areas
A Lounge Area is required for therapeutic and social purposes. These include reading, writing and watching television or videos. The Lounge, Kitchenette and Dining Areas may be combined in a large Multi-purpose Day Room or in separate but adjacent areas.
Service Areas
The service entry is required so that deliveries to the facility do not have to pass through the main entrance of the building. It may also provide ambulance service access and egress in emergency circumstances.
Design considerations include:
- An area large enough to allow vehicles including ambulances to turn and manoeuvre
- A large space with blank wall space for temporary storage of items such as linen or food trolleys, furniture or equipment for repair
- Access to soiled linen should only be available through the service entry or in large institutions separate zones may be available for the various utilities and deliveries
- Adequate infection control
- A loading bay that gives access for delivery staff and staff loading equipment and mobility aids into vehicles, located away from the client entry point.
Wheelchair Parking
An area should be provided near the entrance for parking wheelchairs and electric scooters. The wheelchair parking area requires power outlets for recharging of electric wheelchairs and scooters when they are not in use. Cupboards may be provided over wheelchairs for additional storage.
iv) Hydrotherapy Pool
The need for a hydrotherapy pool should be carefully considered. The cost per unit of treatment is high and conditions for which hydrotherapy is the only appropriate treatment are limited.
Hydrotherapy pools should only be provided where patient numbers are appropriate and where the pool is required for a minimum of four hours per day, five days per week.
Pool Size
The recommended pool size is 7500mm x 4500mm. A rectangular shape is recommended, with the length of the pool generally one and a half times the width.
Pool Depth
To optimise the use of a pool for therapeutic purposes, consideration should be given to the average height of both the smallest users and the tallest users. The recommended minimum depth is 800mm at the shallow end and the maximum depth is 1500mm at the deep end
Gradient of Pool Floor
The floor of the pool should contain no steps.
Entry to Pool
Steps are the accepted method of entry and exit and can also provide functional training. Steps should be placed at the shallow end of the pool and should not intrude into the working area of the pool.
A hoist should be provided and placed at a depth where the therapist can stand and maintain body balance to float the patient off and on the hoist without difficulty.
Temperature
The water temperature should be maintained in the range of 30 to 35 degrees Celsius with an optimum temperature of 34-35 degrees for most conditions being treated. The ambient temperature should be lower than the water temperature for comfort of pool side staff and patients.
Humidity control needs to be provided to minimise condensation. A pool cover may be considered to assist in maintaining water temperature and to reduce heating costs.
Reflection
The lighting should allow the floor of the pool to be seen and should minimise reflection / glare off the surface of the water.
Pool Surrounds
Non-slip surfaces shall be used for the pool surrounds. Ample space should be provided around the pool for staff and patient movements as well as to provide space for patients who are waiting to enter the pool or relaxing after leaving the pool. The building structure, including all fittings, should be rust-proof.
Change Facilities
Change facilities will be required for patients and staff; the size will be dependent upon the size of the pool and the expected number of users.
Emergency Call System
Adequate emergency call points should be provided. Emergency call points should also be accessible from the concourse area and from within the pool.
Plant room
A Plant Room will be required for water treatment plant and any associated equipment.
Footbaths / Showers
Footbaths, foot sprays or showers may be considered in the design of the pool area.
Security
Security design should address:
- Personal security of patients and staff
- Property security of patients and staff
- Unit premises and equipment
- Emergency access and egress
Storage
Design should address the following storage requirements:
- Therapy equipment
- Consumables, and pool supplies
- Pool aids and exercise equipment
- Personal property of patient and staff
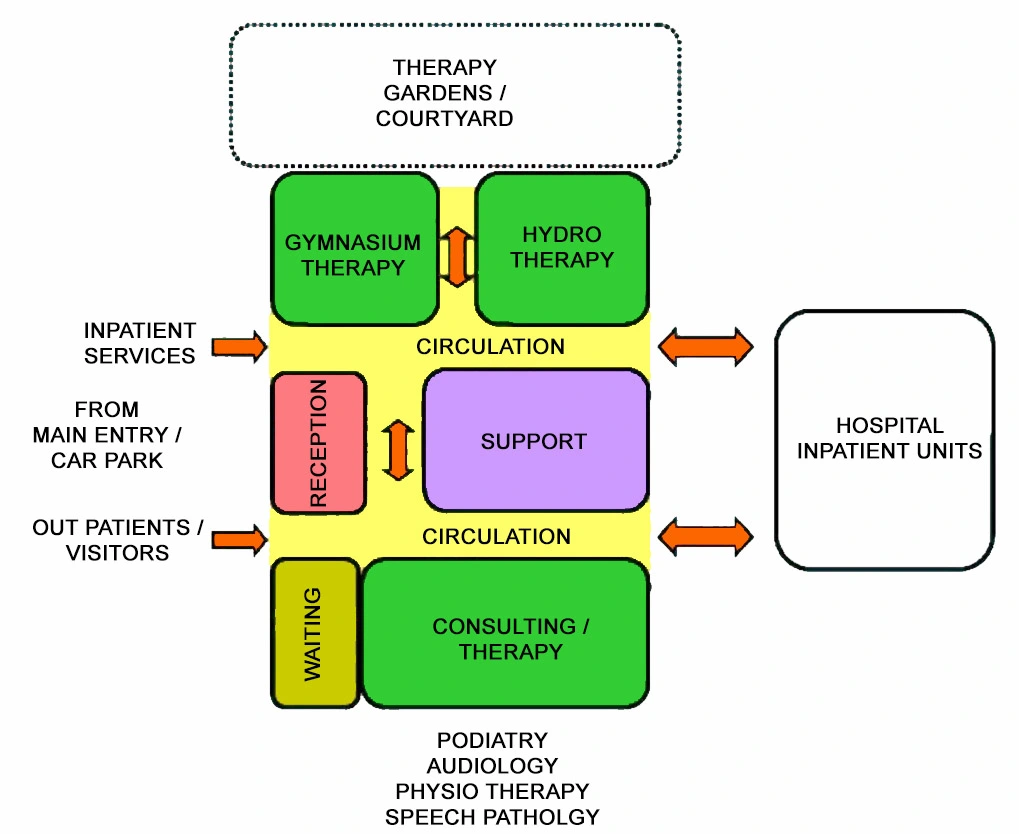
v) Functional Relationships
The most critical relationship in circumstances where Rehabilitation Medicine is an established service is with its own Inpatient Unit/s. However, consideration must also be given to necessary relationships with those units most utilising therapy services in terms of the logistics of patient travel and transport.
In some instances there may need to be duplication of facilities. The Unit should have ready access to allied health units such as speech pathology, social work and the like where those units are not represented or located within the Unit itself. Physiotherapy areas will require ready access to Orthopaedic Clinics.
3) Design of Rehabilitation – Allied Health Unit
i) General
The design philosophy of the Rehabilitation Unit should convey a friendly and inviting environment and should encourage community members to utilise the available facilities for rehabilitation purposes.
A non-institutional, safe and supportive environment needs to be promoted. Building design must be flexible and adaptable to enable the unit to cater for varying client and service needs.
Buildings should be designed to cope with a wide range of possible conditions. The aim is to provide an environment that will allow the maximum mobility possible for each person. The Rehabilitation Unit will include access for disabled persons.
ii) Accessibility
External
If at ground floor unit with its own entry, an undercover set-down bay should be provided at the entrance to the Unit for those outpatients who arrive by bus or car and for return of loan equipment with parking for people with disabilities. Access to other units in the facility should be convenient and covered.
Internal
The Unit should be accessible from the inside hospital’s main entrance. Wheelchair access is required to all patient accessed areas of the Unit. Access equipment is desirable.
Parking
Drop-off and parking for people with disabilities is recommended.
iii) Environmental Considerations
Acoustics
The majority of the therapy areas of the Unit are open space. Further, the activities undertaken therein require hard, impervious flooring (timber or sheet vinyl) and generate noise.
Other areas within the Unit require acoustic privacy in order to be effective or prevent embarrassment such as Respiratory Treatment Rooms and rooms used for women’s health disorders.
Account should be taken of the potential sources of noise within as well as from outside the Unit. Solutions to the various acoustic characteristics and requirements include:
- Use of curtains and other soft fabrics
- Use of solid core doors
- Co-locate potentially noisy areas
- Strategic positioning of storage areas to create a sound buffer
- Carpet in patient areas is not recommended.
- Speech Pathology rooms have specific requirements in order to operate effectively.
Please refer to () “Acoustic Solutions for Healthcare Facilities”
Lighting
Natural lighting is essential in large treatment areas such as gymnasiums and in Staff Rooms. Consideration should be given to lighting levels for patients who are visually impaired.
Climate Control
Good temperature control and ventilation in treatment areas as work can be arduous for both patients and staff. It is important to remember that certain patients such as those with spinal cord injuries are unable to regulate their body temperature.
It is therefore imperative that the gymnasium is air-conditioned. Regardless of orientation, there must be means of sun control.
Interior Design
The rehabilitation process is often a long one with patients commencing attendance at the Unit as inpatients and continuing as outpatients.
Consequently, the Unit should seek to provide a welcoming and supportive environment as it is essential that patients feel positive about returning to the Unit on a regular basis.
iv) Space Standards and Components
Some examples of the average circulation space sizes required for ambulant people using the following mobility aids are:
- One person using a walking stick – 750 mm width
- One person using elbow crutches – 900 mm width
- One person using two walking sticks – 800 mm width
- One person using crutches – 950 mm width
- One person using walking frame – 900 mm width
v) Safety & Security
Safety
The patient population of this unit in particular requires special consideration in terms of safety as they will be at once disabled or incapacitated and yet are being encouraged to be mobile and self-sufficient.
Every aspect of unit design with regard to finishes, surfaces and fittings must be assessed to determine the potential for accidents or hazards to both patients and staff. Sanitary facilities are where most accidents or mishaps occur, to both patients and staff.
In particular, consider:
- Slippery or wet floors
- Protrusions or sharp edges
- Stability and height of equipment or fittings
- Choice of floor covering
- Handrails and wheelchair access are mandatory.
Security
Security aspects should be considered for after hours access control if used by the general public for classes, eg hydrotherapy.
vi) Finishes
It is essential that floor finishes are non-slip and do not create “drag” for patients using walking aids and wheelchairs. Refer also to () of these Guidelines.
vii) Fixtures & Fittings
Height of light switches need to abide by accessibility codes. Handrails on both sides of corridors are recommended.
Also refer to part C of these Guidelines and to the Room Data Sheets (RDS) and Room Layout Sheets (RLS) for further detailed information
viii) Building Services Requirements
Information Technology and Management
IT infrastructure must be compatible with overall hospital systems. There must be sufficient data points and power for computers and student laptops for direct entry of electronic records in the future and for viewing of digital images. (PACS).
Duress Alarm System
Locate at Reception and in Treatment Areas.
Nurse & Emergency Call Systems
Nurse call systems in all individual rooms and cubicles including those in Gymnasiums. Staff Assist and Emergency Call at regular intervals. Annunciators (non-scrolling) located in Reception, corridors, treatment areas and Staff Room.
4) Components of the Unit
i) General
The Rehabilitation – Allied Health Unit will contain a combination of Standard Components and Non-Standard Components. Provide Standard Components to comply with details in the Standard Components described in these Guidelines. Refer also to Standard Components Room Data Sheets and Room Layout Sheets.
ii) Non Standard Components
ADL Computer room
Description and Function – The ADL Computer Room provides an area for activities of daily living (ADL) patient assessment and training for computer activities. A range of variable height computer desks will be included. Doors to this room are optional.
Location and Relationships – The ADL computer room may be located adjacent to the ADL Lounge or other ADL assessment areas.
Considerations – Provide adjustable height computer workstations with the following:
- A variety of desktop and laptop computers
- Printer and telephone
- Power and data outlets for each
Bay – Drinking water
Description and Function – The Bay – Drinking Water provides a recessed area for a drinking water unit.
Location and Relationships – The bay will be located in public access areas close to Waiting areas.
Considerations – The Bay will include:
- Wall and floor finishes suitable for wet areas
- Drinking water fountain, with hydraulic connection to drinking water
- Fittings may include a dispenser for cups and waste bin.
Occupational Therapy / Workshop rooms
Description and Function – The Occupational Therapy Rooms are large spaces provided to enable a range of static and dynamic activities to take place.
The rooms may include space for table based activities, such as upper limb activities or functional mobility activities such as woodwork or splinting activities in a workshop environment.
The Rooms area will be sized according to the number of patients to be accommodated, the activities to be undertaken and will be dependant on Operational Policy and service demand.
Location and Relationships – The Occupational Therapy area may be located adjacent to rehabilitation therapy areas, with ready access to waiting and amenities areas.
Considerations – Fittings and Equipment required in this area may include:
- Benches with inset sink, wheelchair accessible
- Shelving for storage of equipment or tools
- Tables, adjustable height
- Chairs, adjustable height
- Hand-washing basin with liquid soap and paper towel fittings
- Pinboard and whiteboard for displays
- Sufficient GPOs for equipment or tools to be used in activity areas
Workshop areas will require suitable air extraction and exhaust for woodwork activities.
Optical Shop
Description/ Function – An Optical Shop is where clients and patients can have eye tests and purchase prescribed spectacles. It has a combined clinical and retail function.
Location and Relationships – The Optical Shop shall be located near the main entry and among other retail outlets if provided within a larger facility. A glazed shop-front is recommended and shall be positioned next to the major traffic (main corridor).
Considerations – The following areas and functions shall be included in an optical shop:
- Large and well-lit open plan area with display cabinets including a small counter for cashier and paperwork
- A consult room for eye test including slit lamp, light box (or projector for projected image), handwashing basin, drug refrigerator etc.
- Workroom for fitting/ adjusting spectacles
- Facilities for disinfection, sterilisation and instruments reprocessing if required by the Operational Policy
- An office for the optometrist (or can be part of the consult room if sufficient space is provided)
- Storage for spectacles, patient records, stationery etc.
- Access to toilet facilities (can be shared if located in a larger premise)
Plant room – Water Treatment
Description/ Function – The Water Treatment Plant Room is a lockable room for water treatment plant equipment used in the hydrotherapy pool and may include booster pumps and filters. Plant equipment must be installed according to manufacturer’s specifications.
Location and Relationships – The Water Treatment Plant Room should be located in close proximity to the Hydrotherapy Pool with easy access for staff to monitor and service the water treatment systems.
Considerations – Design Requirements include the following:
- Ventilation, exhaust and/or airconditioning must be designed to accommodate the heat loads of the specified equipment
- High level sound isolation is required to ensure noise generated from this room does not invade the pool area
- Structural Engineer’s assessment must be sought for floor load bearing capacity with respect to water treatment plant equipment
- Service access will be required around the perimeter of all plant equipment
- The room will require drainage
5) Schedule of Accommodation
Rehabilitation – Allied Health Unit Generic Schedule of Accommodation
Schedule of Accommodation for a Rehab – Allied Health Unit for Levels 4-6
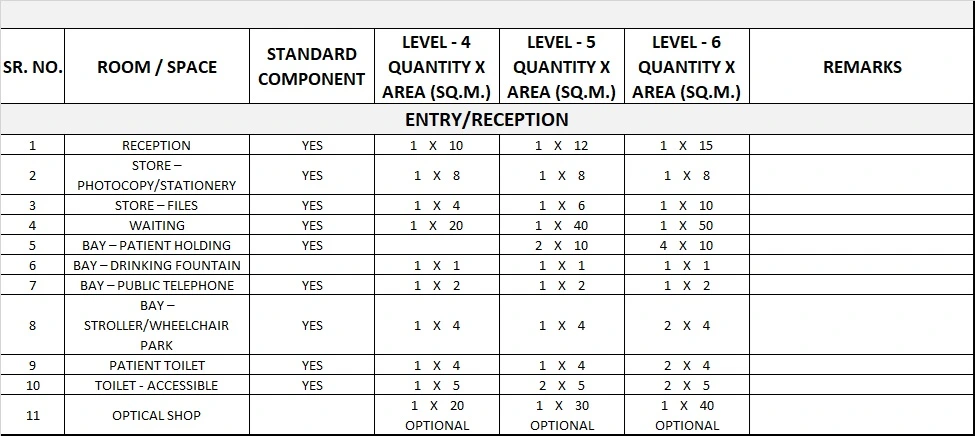
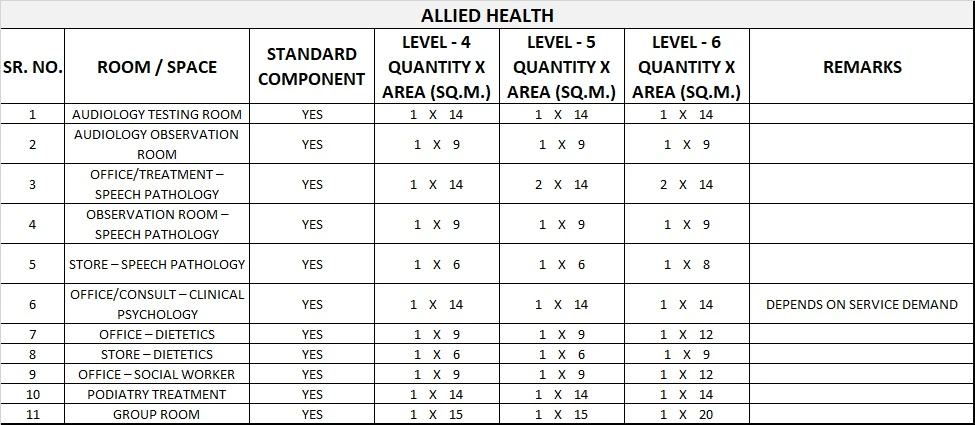
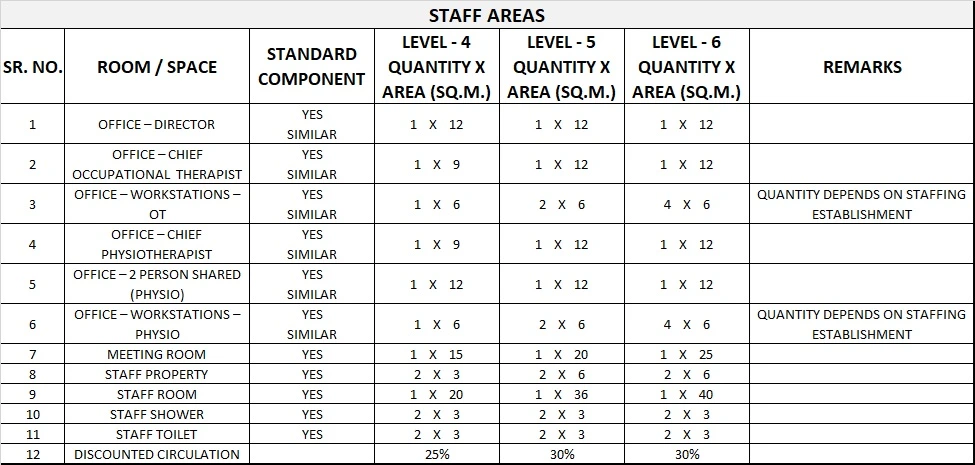
Please note the following:
- Areas noted in Schedules of Accommodation take precedence over all other areas noted in the FPU.
- Rooms indicated in the schedule reflect the typical arrangement according to the Role Delineation.
- Exact requirements for room quantities and sizes will reflect Key Planning Units identified in the service plan and the policies of the Unit.
- Room sizes indicated should be viewed as a minimum requirement; variations are acceptable to reflect the needs of individual Unit.
- Office areas are to be provided according to the Unit role delineation and staffing establishment.
- Staff and support rooms may be shared between Functional Planning Units dependant on location and accessibility to each unit and may provide scope to reduce duplication of facilities.
6) Functional Relationship Diagram
Rehabilitation – Allied Health Unit Functional Relationship Diagram